Get our latest book recommendations, author news, competitions, offers, and other information right to your inbox.
Table of Contents
About The Book
For Dr. Jessi Gold, everything was absolutely fine—until it suddenly wasn’t. As an assistant professor, practicing psychiatrist, university wellness leader, regular media expert, and dedicated friend and family member, Jessi was used to being constantly busy. After all, people—her patients, colleagues, and loved ones—needed her, so who was she to say no to any opportunity to help, be that an extra therapy session, corporate wellness talk, or favor for a friend. She was a doctor, trained to serve, to put the needs of others before her own. But when Jessi is so mentally overwhelmed that she commits an unthinkable error during a patient session, she’s forced to reevaluate everything that the medical system has taught her.
While reassessing her own complex relationship to the health-care industry, Jessi begins to examine it through the eyes of some of her healthcare worker patients—a thirty-something resident with OCD, a pregnant nurse suffering from PTSD, an aspiring medical student with crippling test anxiety, and an experienced ER physician who feels completely overwhelmed. In their discussions of burnout, perfectionism, empathy, and the emotional burden of working in health care, and through her own personal therapy sessions, Jessi recognizes that she is not alone in struggling to maintain her humanity, in a field that she chose because of its humanity in the first place.
Expertly weaving research expertise with unforgettable stories and raw emotion, How Do You Feel? demonstrates the unbridled capacity that we as humans have for connecting, learning, and growing. At once deeply personal, but also utterly universal, it reminds us all that when caring for others, we first have to remember to care for ourselves.
Reading Group Guide
Get a FREE ebook by joining our mailing list today! Get our latest book recommendations, author news, competitions, offers, and other information right to your inbox.
Discussion Questions:
1. HOW DO YOU FEEL? begins with Gold sharing an uncomfortable moment during a session with a patient. How does this set the tone for the rest of the book? Why do you think she chose this scene to open the book with? (For people in healthcare: If something similar happened to you, do you think you would have reacted the same?)
2. Gold struggles with the fact that, during the pandemic, she is considered a “non-essential” worker. How does this impact her sense of identity as a healthcare worker and her job of taking care of healthcare workers who are on the frontlines? Discuss the moment where she struggles to go into the hospital when she’s on call. What do you think about her decision to include this, and why do you think she did even though it might not be something most people not have admitted? (For people in healthcare: Thinking back to that time for you, did you ever question your identity or role? How did you feel about it?) Knowing what we know now post-pandemic, do you think healthcare workers in psychiatry would be treated the same way if another pandemic hit?
3. Throughout the book, Gold talks about the idea that healthcare workers, starting from their early days in school and prepping for the MCAT, define themselves by their career path. Why do you think this is the case, particularly in healthcare, and what toll does this take on them? How is this different from other industries and career trajectories?
4. Gold shares that she was an “overachiever” growing up and always strove to accomplish many goals and wear many hats. How do you think this affected her as she went through the pre-medical journey and started work in psychiatry? Do you think being an “overachiever” is something that has impacted you in your field, whether you work in healthcare or not? How so?
5. Gold writes that there are two types of perfectionism: adaptive and maladaptive. What did that discussion make you think of your own behaviors? Knowing this, would you still want your doctor to be one?
6. Presenteeism is the opposite of absenteeism and is very common in our workplaces. Gold tells a few stories about what she has heard and seen in medicine about this. What is it like in your own field? Do you feel like you can really take time off when you are sick, or if you need a mental health day? Why or why not?
7. Throughout the book, Gold’s relationship with her own therapist, Dr. Miller, is discussed. How does Gold’s relationship with Dr. Miller help her to uncover truths about herself? How does the discussion of their relationship, parallel to Gold’s discussion of what she is going through as a healthcare provider, impact the reader’s experience?
8. Self-disclosing (when a therapist shares information about themself to a patient) is talked about many times throughout the book. Gold discusses how, although it’s often not encouraged, she has found it to be sometimes helpful in building trust with a patient. What do you think about this? How much self-disclosing do you think is appropriate by a doctor, but especially a mental health provider? Do you think it would (or, has it) affected your relationship with a therapist? What do you think about Gold choosing to write a memoir, given these conversations?
9. Gold chose to feature the stories of four “patients” in the book to help share her story. Do you think this choice was helpful in your reading of the book? Why might Gold have decided to include patient examples rather than strictly outline her own experiences? Did one of these patients stand out to you in particular? Why?
10. On page 234, Megan shares with Dr. Gold the story of one of her patients commending her for crying when her husband had passed, sharing that it helped her deeply. In response, Gold wonders if it’s “okay to be a psychiatrist who cries in front of colleagues or patients.” What do you think? Is there a difference between a hospital doctor and a psychiatrist showing this type of emotional vulnerability? Why or why not? Do you think it is appropriate to show emotions in any workplace? What kind of messages have you received, explicit or otherwise, in your own field about sharing your feelings?
11. Gold discusses the toll that the Covid pandemic takes on her, and specifically on her telehealth appointments. On the patient end, how do you feel about telehealth? Do you agree that it can lead to a less personal, connected experience between the healthcare worker and the patient? What are the pros and cons of telehealth, especially as it seems to be a more permanent fixture in post-Covid healthcare?
10. If you work in healthcare: do you relate to any of Gold’s story? Have you felt that you need to suppress human emotion in order to serve your patients? What messages did you get in school and training about them? How do you think this has impacted you and your patient care? Does reading Gold’s story make you think any differently about your experience or your own mental health? If you don’t work in healthcare, do you feel you understand healthcare workers better after reading HOW DO YOU FEEL?
11. Gold discusses that many of the issues she has with healthcare culture are large, systemic ones, which might feel overwhelming to think about. What are some ways, on a day-to-day level, that you think individuals can help to combat the stigmas that Gold outlines throughout the book? What kinds of skills that Gold describes trying herself or discusses with her patients resonate with you or have worked for you in the past?
13. If you have been or currently are in therapy or psychiatry: What did you appreciate about Gold’s vulnerability in sharing her struggles as a therapist? Does this affect the way you might think about your own treatment? Do you think there is a different stigma associated with medications vs. therapy? Why?
14. If you have not been in therapy or psychiatry: Do you have a different perspective of therapy now? Do you think the ideas Gold discussed can apply at all to your life or your line of work?
14. Why do you think Gold chose HOW DO YOU FEEL? as the title? What is its significance in the book as a whole?
Activities
1. Pick a scene or “patient” described in the book and act out what a conversation between them and their therapist might be. Try to really embody) the characters and imagine how they might be feeling. Then, debrief and discuss how you felt, or what insights you might have gained, acting this out.
2. Take a few moments to self-reflect or journal, individually, about how you related (or didn’t relate) to the book. This can include how you cope with your emotions at work, or how the Covid pandemic affected you emotionally. Share and discuss as a group.
3. Pick a study that Dr. Gold referenced in the book which piqued your interest and read further about it. Then, present your findings to the group.
4. Dr. Gold shares a lot about the role of poetry and music in her own mental health and how sometimes she chooses other people’s words to better describe her own. Pick a song or poem or meme that helps you express your mental health, and explain why.
Author Q&A
HOW DO YOU FEEL? begins with you hitting what you describe as a “breaking point.” How did you get there? What did the lead-up to that moment look like?
Sometimes you don’t know you’re off until you’re REALLY off. Like so many of my patients, I blow past early warning signs (for me, extreme anger at my inbox, for example), and attribute them to work or, really, medicine just being hard. I think “I’m fine” and just “a little tired,” and push through nearly falling asleep, and ignore my emotions, and just keep going. I learned to do that in medical school, because we’re always needed, and not supposed to come first, and all of those thoughts were only compounded in the pandemic. I felt pulled and needed so much as a psychiatrist who saw healthcare workers and an administrator in charge of our staff and faculty support during such a challenging time, but I also felt guilty because I was not an “actual frontline worker” and that only made me want to do more and more. What feels like a sudden break is never really sudden, but is often just bad enough for you to finally recognize yourself in the equation.
This book discusses not only the challenges healthcare workers face but also the complexities of caring for others in general. What implications do your findings have for readers who are outside of the medical field but are nonetheless struggling with the difficulties of care work in their personal lives?
Not everyone is in healthcare, but healthcare is just one example of putting others before yourself. Take motherhood, instead: I hear over and over from women that they care for their kids, and sometimes also their parents, and after that, there is no time for them. The truth is, we are all better caregivers when we recognize and take care of our own needs. I think seeing me and the patients in the book struggle with this balance is not only validating but enlightening. I hope people who struggle with the same universal themes (overwork, perfectionism, empathy, burnout) feel less alone, but also learn some tips and tricks to try in their own lives. It isn’t a self-help book, but readers will see me suggest interventions to my patients and my therapist do the same to me, and can decide if they want to incorporate any of those ideas into their lives. Plus, if a healthcare worker who studies mental health topics like burnout (or, in the case of me, specializes in it!) can fail to notice symptoms in themselves, or better yet, stigmatizes mental health conditions, of course everyone else does. It puts into perspective just how challenging it is to prioritize our mental health, and that itself is a worthwhile conversation to have out loud.
HOW DO YOU FEEL? recounts sessions with four of your healthcare worker patients. How did working with these patients affect your understanding of the issues in which you specialize—and even your understanding of what you were experiencing on a personal level?
I fell in love with psychiatry because of patients’ stories. I loved how I could hear a hundred stories of people with depression, and maybe their medication treatment would be similar, but the reasons for their depression were always different. Every day I learn something from the privilege of sitting with patients and being the first (and often only) person they tell some of their hardest life challenges. Sometimes my understanding grows just because of how they describe their subjective experience, or the culture of healthcare in their fears and opinions, and that informs how I help them and other patients like them in the future. But, also, their stories can trigger something in me—a memory, or a similar feeling or thought—and that often means something deeper. I might journal or ruminate on it, or, better yet, bring it with me to therapy and that reflection, of my feelings because of a patient, can help me learn more about myself as a result.
Some readers may be surprised to learn that healthcare workers like you navigate many of the same issues they do when it comes to seeking care and connecting with a therapist. You mention that those trained in mental health, like most people, sometimes lie to their therapists. What’s behind this? Why do so many of us struggle with total honesty even in this ostensible safe space?
Being a psychiatrist in therapy is just like everyone else being in therapy, except I have training in it. That adds a sort of meta layer to our relationship where I can sometimes notice communication techniques and my own resistance, and perhaps that makes me a little more annoying as a client (and not everyone would choose me as one!). Still, noticing I’m doing something doesn’t necessarily mean I don’t do it. Case in point—I’ve lied to my therapist (not the one in the book, though, she’s special). We lie because we aren’t ready to have those conversations yet, or we’re afraid of being judged (even if it is a safe space), because others have judged us before or we’ve seen someone else be judged for something similar. In truth, though, we have to get through the scary stuff out loud to fully process it. Sometimes it feels safer to leave it in a box on a shelf and avoid it, but the box always gets heavy and breaks eventually.
HOW DO YOU FEEL? pulls back the curtain on many less-discussed aspects of providing mental health treatment, including by detailing the complex emotions you’re navigating during your sessions with patients. These reflections are often vulnerable—you reveal that therapists sometimes struggle to maintain detachment, experience self-protective impulses, find themselves heading into a session in a state of agitation, and worry about avoiding secondary trauma. Why was it important to you to reveal the more tangly aspects of the practitioner’s experience?
Psychiatrists don’t often have the best reputation to the public. Maybe because of Freud our silence comes off as uncaring, and maybe because of people’s bad experiences with one doctor or another, we now have a reputation for just being drug pushers, and not curious about patients’ stories. But, in my experience, all of that couldn’t be further from the truth. By pulling back the curtain, quite literally into my own head, I wanted not just to show people what we do but also to emphasize our humanity. The latter is important for both patients and mental health practitioners to recognize. Too often we pretend our jobs don’t affect us, and that to truly do our jobs well, they can’t. But that is a myth. I often think about a quote by Rachel Ramen: “The expectation that we can be immersed in suffering and loss daily and not be touched by it is as unrealistic as expecting to be able to walk through water without getting wet.” I think it’s about time we talk about the water, and what it feels like to be constantly rained on. Silence isn’t helping anyone.
You’ve become an authoritative voice in the media on burnout, an issue you also address with patients in your clinical practice. How did you come to develop that niche?
I didn’t wake up one day and decide to be a burnout expert, but it more or less found me. When I was in college, I started to observe that people in pre-med who were kind, not cutthroat, and would have made awesome doctors, regularly dropped out. I became so curious about why, that I studied pre-med as a culture for my Master's thesis in Anthropology. After that, once my eyes were open to some of these challenges and disparities, they were constantly aware. I studied med student mental health and access to care in medical school, and started (and helped lead) support groups for medical students as a resident. Aware that burnout was a major issue I was hearing about in all levels of training even before the pandemic, in March 2020, I had the background to jump in quickly and help. I was clinically seeing healthcare workers, students, faculty, and staff, and also working on outreach and education. At the same time, noticing the same issues across the country, I was talking about it in writing (e.g. I wrote a STAT piece on it in April 2020 long before it was covered elsewhere) and on social media. COVID didn’t create the mental health crisis in healthcare, so it doesn’t stop just because COVID did. It is my job to remind people of that.
You disclose that you experienced burnout yourself. What pushes healthcare workers towards burnout? What are some of the warning signs? What coping mechanism did you employ to handle burnout? What advice would you give to others experiencing burnout?
Burnout is a workplace associated condition, meaning that the systems and circumstances where you work, caused you to feel the symptoms you experience. In healthcare, the reasons for burnout are vast and include everything from documentation and electronic medical records, to insurance companies and safety in the workplace, to a general lack of support. It is no wonder that doctors are burned out at rates as high as 50%, and more than other fields. Burnout is not simply “being tired from work”, but is defined as 3 different overall symptoms: 1) Emotional exhaustion: This looks a lot like physical exhaustion but you just feel “done” at the end of a workday 2) Depersonalization (or Cynicism depending who you ask): Feeling disconnected or more angry/frustrated, and 3) A reduced sense of personal accomplishment, which is more self-explanatory. In my practice, and personal experience, the first 2 symptoms are often blown past and ignored as predictable outcomes of work, especially in medicine where the baseline is basically to not sleep, not eat, and be burned out, but once someone feels they are doing less, or someone else might think they are doing less, they start to take notice.
This means, though, that the more subtle symptoms, like overwhelm, a change in your schedule, or procrastination, are often ignored and it is more severe by the time you pay attention and try to take action, which happened to me (and so many of my patients!). By that time, time off is really all that can help and allow you a break and reset, as something like yoga will feel useless, and even detrimental as a suggestion, at that time. Once I reset, though, it was important that I didn’t just go back to the same ways of coping with a bad system that I did initially. One of the things that helps now is paying more attention and asking myself how I am feeling regularly, and not just when things are bad. Not only does it remind me I am part of the equation and might have reactions, it lets me notice changes earlier, with more options for interventions to help. I tell this to anyone who asks, as a good place to start: So, how do you feel?
What systemic changes would you like to see to help prevent burnout? How can supervisors identify and better assist someone who might be struggling?
Across the board in studies the things that help with burnout are meaning, purpose, and supportive supervisors. Meaning and purpose can feel intangible and philosophical even, but what it really means is when we spend more of our time mentoring or seeing patients (what we signed up to do, and derive meaning from) instead of paperwork and charting and yelling at insurance companies, we feel less burned out. To do this, systems need to look at what is in place to support their healthcare workers- other staff, time off, changes to the electronic medical records- and invest in helping their teams spend more time on their purpose. The concept of a “supportive supervisor” is vague, in some sense, but has to do with communication, transparency, and the culture in the workplace. Supervisors need to be trained to recognize burnout and talk about burnout with their teams, but also in how to create supportive work environments. The good ones should be rewarded, often, and others should be given education and skills to help their behaviors. Policies, like leave and remote work, come into play here as well- as a more flexible workplace that supports work/life balance will lead to less burnout. Ultimately, every area of the system interacts with burnout in some way, which is why jobs like mine, as a Chief Wellness Officer, even exist. We can be the ones to work across the silos, and remind people of the humanity of the workforce every chance we get.
How do you feel?
Anxious and even a little afraid, but also proud and excited—like any good expression of vulnerability.
Product Details
- Publisher: S&S/Simon Element (November 7, 2024)
- Length: 288 pages
- ISBN13: 9781982199777
Browse Related Books
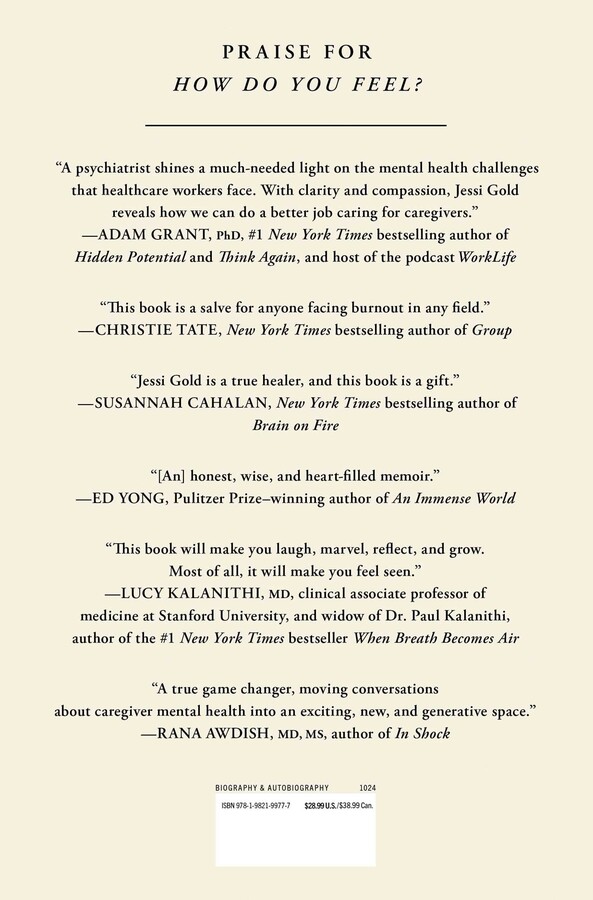
Raves and Reviews
"A psychiatrist shines a much-needed light on the mental health challenges that healthcare workers face. With clarity and compassion, Jessi Gold reveals how we can do a better job caring for caregivers." –Adam Grant, PHD, #1 New York Times bestselling author of HIDDEN POTENTIAL and THINK AGAIN, and host of the podcast WorkLife
“Raw and touching… It’s an eye-opener." -Publisher's Weekly
"In How Do You Feel? Jessi Gold, M.D., opens a compassionate, intelligent portal into the lives of the healthcare workers struggling with their own mental health. Gold's deep-dive into the human psyches of those who serve others in the healthcare industry illuminates how difficult it is for the helpers among us to get help for themselves. With the perfect blend of stories from her practice, science, and personal narrative, Gold sheds light on the price healthcare workers pay for neglecting themselves and breaks through the stigma that keeps so many of them silent. This book is a salve for anyone facing burnout in any field, and Gold is the best kind of guide: warm, witty, and genuinely invested in other people's lives. " —Christie Tate, New York Times bestselling author of Group
“In this honest, wise, and heart-filled memoir, Jessi Gold reveals what it takes to retain the humanity that medicine so often forces doctors to set aside, and what it means to help yourself while helping others. I loved this book, both as a journalist who has tried to provide a similar kind of service and as a patient who has sought help from therapy." — Ed Yong, Pulitzer-Prize winning author of An Immense World
“Raw and touching… It’s an eye-opener." -Publisher's Weekly
"How Do You Feel? is a compelling, courageous, and portrait of a psychiatrist. I've never read such an open-hearted and honest account of what it takes to work in mental health care today. This is an ode to the art of clinical care—a paean to empathy. Jessi Gold is a true healer and this book is a gift." —Susannah Cahalan, New York Times bestselling author of Brain on Fire
“If you’ve ever said “I’m fine” when you weren’t. If you’ve ever been so many things to so many people that you became unavailable to yourself. If you’ve ever believed you were too much, not nearly enough, or somehow, inexplicably, both at once. This book is for you. For us. Jessi Gold’s How Do You Feel? is one of the most human, most reassuring books I’ve ever read about the intersection of mental health, work, medicine, and culture. What a gift.” —Maggie Smith, New York Times bestselling author of You Could Make This Place Beautiful
“This book will make you laugh, marvel, reflect and grow. Most of all, it will make you feel seen. Whether you’re a healthcare worker, someone who loves one, someone who sees one, or someone who is struggling, Dr. Jessi Gold’s words — and the many intimate stories here, including her own — will be a balm and a guide.” —Lucy Kalanithi, MD, Clinical associate Professor of medicine, Stanford university, and widow of Dr. Paul Kalanithi, author of When Breath Becomes Air
"How Do You Feel? is a thought-provoking exploration of healing and compassion in the face of adversity. Guided by Dr. Gold’s keen insight and sharp writing, we are afforded a rare glimpse into psychiatry’s inner sanctum. Dr. Gold has an extraordinary understanding of the human condition, and her empathy emanates from the pages. A must-read."—Jen Gunter, MD, New York Times bestselling author of The Menopause Manifesto and The Vagina Bible
"In How Do You Feel, Dr. Gold manages the seemingly impossible. She gently brings healthcare workers into conversation with our sometimes complicated inner worlds, and does this with wisdom, humor and candor. She lovingly nudges us to awareness and acknowledgement of the immense emotional load we’ve carried and holds space for our collective reflection. Ultimately she calls on us to do the most radical thing imaginable: to care for ourselves even as we care for others. A true game-changer, moving conversations about caregiver mental health into an exciting, new and generative space." —Rana Awdish, MS MD Author of In Shock
"This is an important book...for healthcare workers, especially physicians, to read and understand that their messy internal lives are normal...and because Dr. Gold's, dare I say, Jessi's humanity, and by extension, the humanity of healthcare workers everywhere, is apparent, relatable, and just so likeable. This book pierces the armor of the white coat to the very human heart beating within." –Stef Simmons, MD, CMO, Dr. Lorna Breen Heroes' Foundation
Resources and Downloads
High Resolution Images
- Book Cover Image (jpg): How Do You Feel? Hardcover 9781982199777
- Author Photo (jpg): Jessi Gold Elijah Wilkerson(0.1 MB)
Any use of an author photo must include its respective photo credit